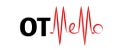
Lab values
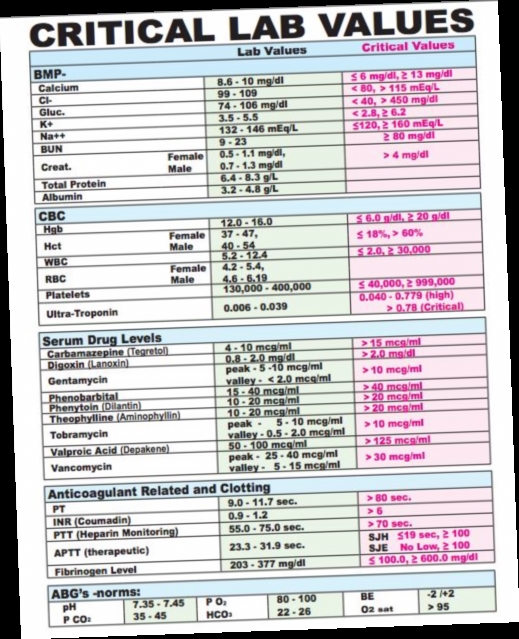
When I was trying to break into acute care, I remember having the impression that knowing lab values was the most significant difference between working in a SNF vs a hospital, which was an oversimplification of the truth. The important things to learn as a new acute care therapist is the role of the staff at the hospital and your role, how to spot red flags in the chart and in person that a patient is not stable to be seen by therapy, and the procedures that the hospital has at it’s disposal to rectify issues.